How much money do junior doctors really earn? If you’ve been listening to the British Medical Association – the trade union which represents junior doctors – this week you will have seen comparisons made between their salaries and the wages of Pret A Manger employees. The union talks about members having to ‘cut back on food and heat to pay bills’. To think of notoriously overworked junior doctors in such circumstances is outrageous. But how typical is that scenario of those demanding a 35 per cent pay rise?
First-year junior doctors are still some of the better-paid workers in Britain, and this is only the jumping-off point
A doctor can be classified as ‘junior’ for years, depending on what type of medicine they practise. Being stuck on a salary of roughly £29,000 per year – the lowest rung on the pay scale – would surely be an injustice, not least because of the unsociable hours and inevitable stress that the job demands. But that isn’t happening, not even for junior doctors in their first year on the job.
The latest figures, for last year, show a typical doctor in their first year of work for NHS England is paid just more than £37,000. This combines the basic pay rate with non-basic pay fees (including working unsociable hours), and adds up to thousands more than the average UK worker is paid. Average earnings for a Foundation Year 2 doctor were just over £43,000 in the same fiscal year, more than £10,000 higher than the average salary.
Is this a banker-level salary? No. But at these levels, first-year junior doctors are still some of the better-paid workers in Britain. And this is only the jumping-off point for doctors’ pay. Get through those first years, and a junior doctor’s pay, based on the latest set of data, approaches double the average wage: doctors classified as being in ‘core training’ or as ‘speciality registrars’ earned, on average, just under £56,000 and £63,000 respectively last year. This is all while still carrying the ‘junior doctor’ title.
Even this does not take in the full picture. For every £10 paid to a junior doctor, the taxpayer contributes £2 to their pension pot – a 20 per cent contribution scheme. The UK average is just under 5 per cent. Both doctors and nurses benefit from this hugely generous pension plan, which is why, when everything is factored in, the average NHS nurse is on a package of £50,000, rising to £60,000 in London. Quite right, you might argue: nurses are some of the most valued people in society. But can we really say that this is not reflected in their remuneration?
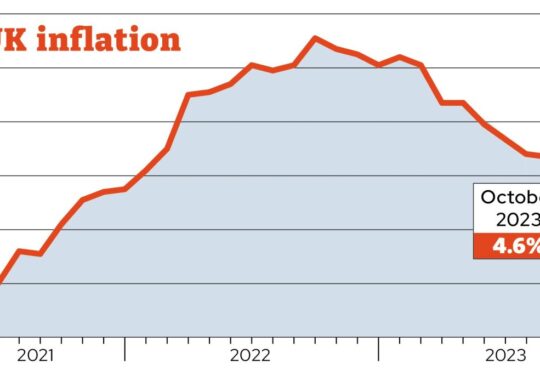
Inflation has without doubt brought misery to millions. But those striking are, comparatively, the well-remunerated. First look at the whole pay package. Then job security. And then lifetime earning
prospects: the average doctor can expect to retire on a personal fortune that stands in enviable comparison with peers in the private or public sectors.
There is a reason last month’s Budget from Jeremy Hunt removed the ‘lifetime allowance’ on pensions in a bid to keep more doctors in the NHS: very few professions see workers earn enough (and get such big pension top-ups) to come near a £1 million pension pot limit. Again, this is not to say that doctors don’t deserve their money: every society needs to lure the best and brightest into the health service. But are doctors really treated so unfairly that they can justify a four-day strike (after a bank holiday) which cancels an estimated 350,000 appointments?
One of the leaders of the junior doctor strikes has been away on holiday this week, an odd priority for someone spearheading a would-be revolution. There’s a feeling inside government that this is the first Gen Z strike, organised by people in their twenties and demanding a 35 per cent rise. That is hard to square with other public priorities, in particular the urgent need to address NHS England’s waiting list of seven million.
While it may be incorrect to say that junior doctors are outrageously underpaid, they are, however – like all other doctors and, indeed, patients – trapped in an often dysfunctional bureaucracy that does sometimes require them to tolerate dangerous conditions. The BMA’s own reporting of the strikes put far more emphasis on the relentless nature of the job: endless night shifts, zero breaks. The shortage of medical staff is a huge problem, as it all but guarantees burnout for the doctors and a less certain quality of care for patients.
Yet the BMA should take responsibility for its role in the UK’s dwindling healthcare workforce. It voted back in 2008 to cap the number of places for medical students in Britain, arguing that an increase of staff risked ‘devaluing the profession’, and, ironically, would make these doctors ‘prey to “unscrupulous profiteers”.’ Fifteen years on, the lack of doctors is being used as leverage to request an off-the-charts pay hike. This is one of the many risks in allowing a monopoly in healthcare, whether it’s state-run or private.

Still, there is a case to be made for junior doctors to get a salary raise – perhaps taking more of their remuneration as salary and less as pension. But it must go hand-in-hand with system reform. There is renewed focus this week on the growing exodus of UK doctors to Europe and Australia in search of better pay and conditions. But many countries’ health systems, while still offering universal access to care, are more marketised than the NHS, increasing the flow of resources that allow for a better life and better pay.
For all the talk of a doctor’s ‘market rate’, the UK does not have any meaningful market in healthcare. This is not by accident, but by design. The consensus for decades has been that the NHS should remain one of the most centralised healthcare systems in the world, with the salaries funded by the taxpayer and its workers classed as ‘public servants’. This may sound attractive in the abstract, but in practice it means lower salaries for workers and worse outcomes for patients.
There is nothing fair about this for either group. But while the junior doctors weigh up their options, it’s the patients who are truly helpless – made to delay their care once again, with nowhere else to turn.